The first “Dementia Village” opened in the Netherlands about 15 years ago. At its heart lies a different paradigm – the creation of neighborhoods, replacing the traditional nursing care institution for residents suffering from severe dementia. Since its inception, dozens of Dementia Villages have been developed, primarily in Europe and Canada. The Hogeweyk® philosophy is based on the deinstitutionalization of care and the emancipation of people living with dementia, providing them with wellbeing by including them in society.
Alexandra Winterstein
16 August 2024
French version | German version
The global increase in the number of dementia cases is staggering. Currently, according to Alzheimer’s Disease International and the World Health Organization, there are about 55 million people affected by dementia today. As our population ages, and we live longer, this number is expected to reach 78 million by 2030. The likelihood is great that each person will have at least one family member or a close friend, who is affected.
It is becoming increasingly obvious that this is a huge challenge for societies, governments and the elderly care industry. While there are many facilities in Europe and the US which specialize in treatment, care and housing for these patients, in the vast majority of cases, the residents are placed in institutional facilities that house several hundreds of people in one building, each accommodation resembling at worst, a hospital room. Excellent nursing care may be provided for, but when one tries to walk in the shoes of someone who has been moved to this residential facility, it is obvious that the final “home” must be an intimidating experience: unfamiliar, unnatural and disorientating. The resident will in all likelihood not understand where or why they are there.
An innovative project known as “Dementia Villages” has been underway for about 15 years. This project has garnered the attention of the media, but is largely invisible to the general population because there are only a few of these villages, they are not widely talked about, and the general public usually does not enter them. And yet, when one thinks about the idea, one can’t help but think that this concept is revolutionary and yet so simple.
The concept behind this inspiring project is the creation of neighborhoods, or small-scale communities for residents, who all suffer from dementia. Dementia is an umbrella term for a usually progressive condition (such as Alzheimer’s disease) marked by the development of multiple cognitive deficits such as memory impairment, aphasia, and the inability to plan and initiate complex behavior.
The first idea for the village came about in 1992 from the management team of Hogeweyk (Yvonne van Amerongen and Jannette Spiering) which was then a traditional nursing home. Van Amerongen, Jannette Spiering and later Eloy van Hal co-created the innovative concept developed specifically for people with severe dementia which was first realized in Weesp in The Netherlands, a small town close to Amsterdam.
Critics have had issues with these villages: the initial investment costs associated with larger spaces, policy support, lack of staffing, a lack of awareness, and some beliefs that residents are living in a happy fantasy world. But is this not much better than living in a hospital room and being treated as sick and infirm? Do these villages fool patients into feeling better, or are they really feeling better?



The Hogeweyk is not a hospital-like building, but is in fact a community composed of Dutch home-like environments: several streets, gardens, shops, a theater, café, and most importantly – small clusters of quaint houses that group approximately 200 residents in neighboring houses. The village looks very much like a regular community – with the exception that all inhabitants share common symptoms of advanced dementia.
Trained staff – doctors, nurses, psychologists and physiotherapists – intermingle seamlessly with the patients. Great care is taken that the traditional nursing home architectural feature, such as crowded corridors, identical rooms, enclosed courtyards, and caregivers dressed in visible medical white or blue scrubs – are conscientiously avoided. Instead, on about four acres, a comfortable, safe, and even healing environment is provided for. It is a safe place – residents can only leave through one exit.
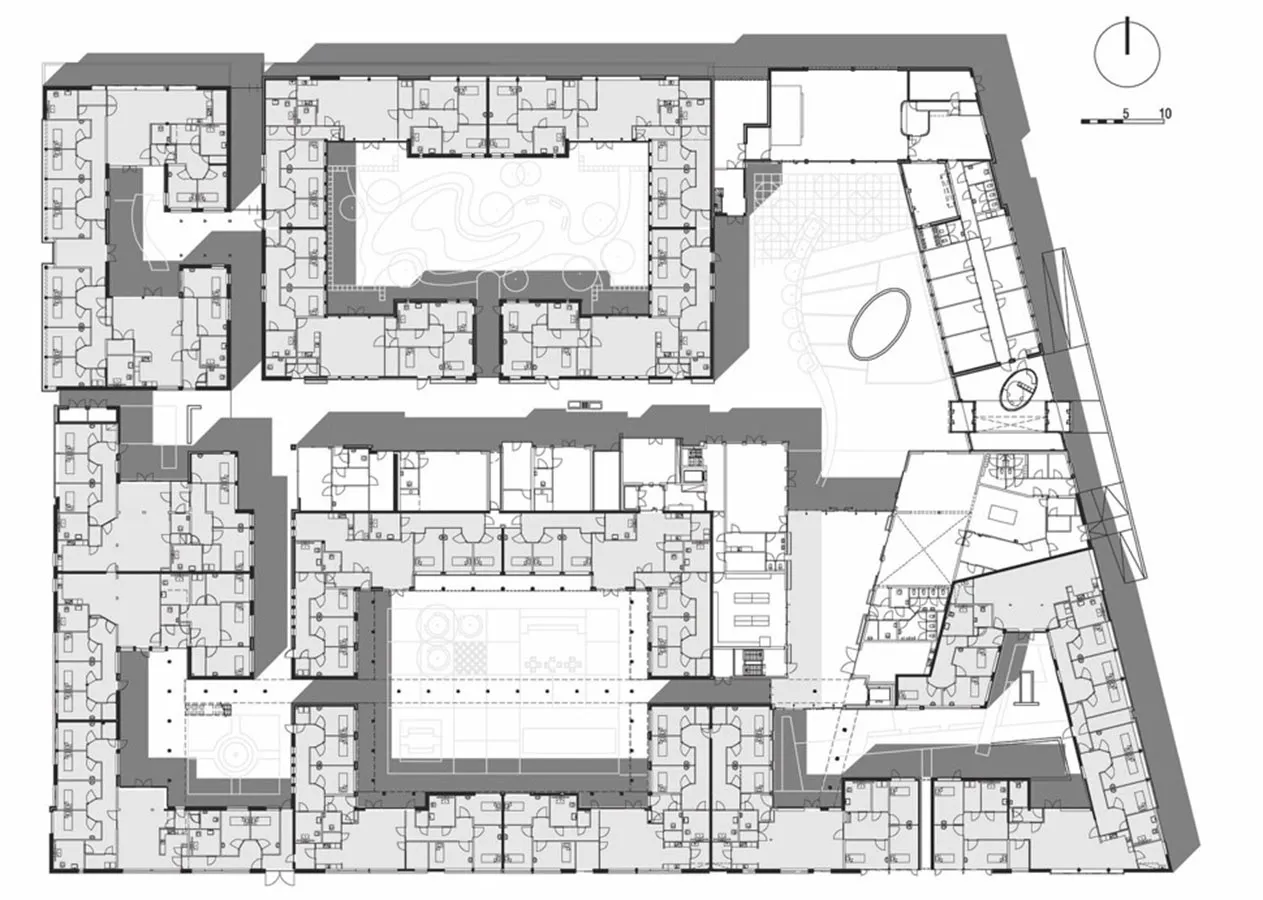 The plan of Hogeweyk, Weesp, Netherlands – the first dementia village. ©The Hogeweyk
The plan of Hogeweyk, Weesp, Netherlands – the first dementia village. ©The Hogeweyk

A unique concept of The Hogeweyk is choice. In traditional care units, a resident may choose to leave their room, but then they immediately find themselves in a shared public space, such as a community room. The resident can choose to go into their own living room, or to leave their apartment for their front yard, or if they decide to be social, they can walk around the village, or go into a public café. Autonomy and independence play a positive role in the residents’ well-being, and there is evidence suggesting that these living models positively impact quality of life. Benefits include reduced anxiety and depression, fewer physical restraints and psychotropic medications, and decreased hospitalizations. Additionally, residents tend to be more engaged and physically active.
Why has this innovative concept not been implemented in more countries?
Dementia Villages can currently be found in Australia, Canada, Denmark, France, Hong Kong, Norway and the UK. In some of these villages, the facilities are open to other local residents in the neighborhood, which has the additional positive effect of reducing stigmatization.
One would think that the greatest obstacle might be funding. A New York Times article from 3 July 2023 entitled “As Cases Soar, “Dementia Villages” Look Like the Future of Home Care” also focused on the exorbitant costs of the system, and that, when available, only the affluent could afford it in countries lacking universal healthcare.
The Hogeweyk, which was primarily funded by the Dutch government and cost slightly over EUR 23 million to build, has been operating at near full capacity since it opened in 2009. The cost of care doesn’t differ from traditional nursing homes. According to Eloy van Hal, who talked to iGlobenews, it does require an open frame of mind and the courage to do things differently: “If you look at the core at what we do, the biggest challenge and difficulty is the culture change from the clinical model to a much more social and holistic model of care and support. This paradigm shift, this change, is the biggest obstacle. Society, including regulations and laws, are often very traditional, medicalized and institutionalized. The Hogeweyk helps to understand that people living in Dutch society and in the world with dementia, have many abilities left, can still learn a lot, and can benefit, but only if not locked away from society.”